The Chances of Getting HIV From One Encounter
What Are The Odds of Getting HIV From a One Night Stand?
Actual Percentages
Author & columnist, featured on HBO, NPR, and in The New York Times
Okay, so your latest hookup just hit you with the news: he's HIV positive. Panic mode, right?
You're probably pacing the floor, mind racing a mile a minute, thinking, 'What are my odds here? Did that one night just throw my life off course?'
This isn't just about a scare; it's about the gnawing, gut-wrenching anxiety that could shadow you for months, maybe even longer, if you don't get a grip on the facts.
So, what's the deal? What are the chances of getting HIV from one encounter? Because let's face it, not knowing whether you should be sprinting to the doc for some post-exposure prophylaxis (PEP) is the kind of uncertainty that can drive anyone to the brink.
Here's your starting point: 1.43%. That's the straight-up probability of contracting HIV from one encounter of receptive anal sex with someone who's positive.
Sounds tiny, doesn't it? But don't let that number fool you into complacency. It's not just about now; it's about every 'what if' that might follow.
In this article, we're diving headfirst into the real, hard numbers—those calculated by the folks who live and breathe this stuff: epidemiologists. They're going to tell us once and for all the chances of getting HIV from one encounter.
But we won't stop there. We're going all in, dissecting how these experts come up with their figures, unraveling the science and stats that lay the groundwork. And because we know life isn't always a one-off, we're also exploring how the risk escalates when you're rolling the dice with unprotected sex on the regular.
This isn't about spreading fear; it's about arming you with knowledge. Because when you know what you're up against, you can make choices that keep you in control. So, buckle up. We're about to take a deep dive into the numbers that could change how you view that 'one night of fun' and what it means for your health moving forward."
The Odds Of Catching HIV From One Encounter
Odds of Getting HIV From a One Night Stand: Top vs Bottom, Oral vs Anal
How HIV Transmission Risk Multiplies with Each New Partner
The Snowball Effect: How Multiple Partners Amplify Your 1.43% HIV Risk
Conditions That Amplify HIV Transmission Risk By 500%
What Are Your Chances of Getting HIV from a Needle Poke?
Unprotected Anal Sex Poses Higher HIV Risk Than Blood-Contaminated Needle Use
What Are the Odds of Catching HIV from a Blood Transfusion?
What Percent of Gay Men Are HIV?
How Experts Determine Your Chances of Catching HIV From One Exposure
Should You Get Post-Exposure Prophylaxis If You Had A One-Night Stand With an HIV Top?
How Many Sexual Partners does the Average Gay Man Have?
What Are The Chances of Getting HIV Sexually? (Our sister article to this one)
Why It's Important For Your Health To Know The Odds of Getting HIV
For many, the fear of HIV is a constant, looming presence, casting a long shadow over everyday life and well-being. It's not just the virus itself that's daunting, but the profound impact it can have on both mental and physical health. Research studies suggest that this constant fear and anxiety of getting HIV contributes to some pretty awful health statistics.
For example, gay men are 300% more likely to experience depression and 113% more likely to suffer from anxiety disorders. The toll on physical health is equally grim, with a 142% higher likelihood of developing Inflammatory Bowel Disease and a 200% increase in the risk of eating disorders.
The impact extends to physical health and addiction, with rates of alcoholism and substance abuse 178% and 122% higher, respectively. Moreover, gay men face a staggering 200% higher risk of homelessness and a heartbreaking 316% increase in the likelihood of suicide.
Getting a grip on the real chances of getting HIV can seriously cut through the fear, and thus reducing some of these negative health outcomes.
It's all about moving from feeling scared and unsure to being in the know and confident. Our guide gets right into it, laying out both the tough parts and the hopeful bits, with one key takeaway: the worry and stress about HIV are real, but armed with the right info and safety steps, you can almost wipe out that fear entirely.
The Likelihood Of Getting HIV From a One Night Stand
Below you'll see the odds ranked from least to most likely:
| Activity | Odds of Catching HIV (One Encounter) |
|---|---|
| Insertive anal sex, no condom, undetectable viral load | 0% |
| Receptive fellatio, no condom, viral load not known | 0% to 0.04% (1 in 2500) |
| Insertive anal sex, no condom | 0.11% (1 in 909) |
| Needlestick injury with contaminated blood | 0.23% (1 in 435) |
| Injecting drug use | 0.63% (1 in 158) |
| Receptive anal sex, no condom | 1.43% (1 in 70) |
Can You Believe How Low These Figures Are?
Wait, the chances of getting hiv in one encounter is just 1.43%? Or LESS?
WTF!
You'd think it was way higher, right? Like 20, 30, or even 40% based on the whispers and rumors floating around. How on earth could it be that low?
This revelation hits like a plot twist in a thriller. It's the kind of stat that makes you pause and rethink everything you thought you knew about the risks of a casual hookup. Experts have been tight-lipped, fearing the fallout of such a low number becoming common knowledge. They worry it might lead to a 'why bother?' attitude towards condoms and PrEP.
But here's the thing. You can't just take that 1.43% at face value and think it applies across the board for every fling. There's more to the story, and a single graph is about to lay it all bare. Brace yourself for a curveball that will change the way you view those supposed one-off risks.
How HIV Transmission Risk Multiplies with Each New Partner
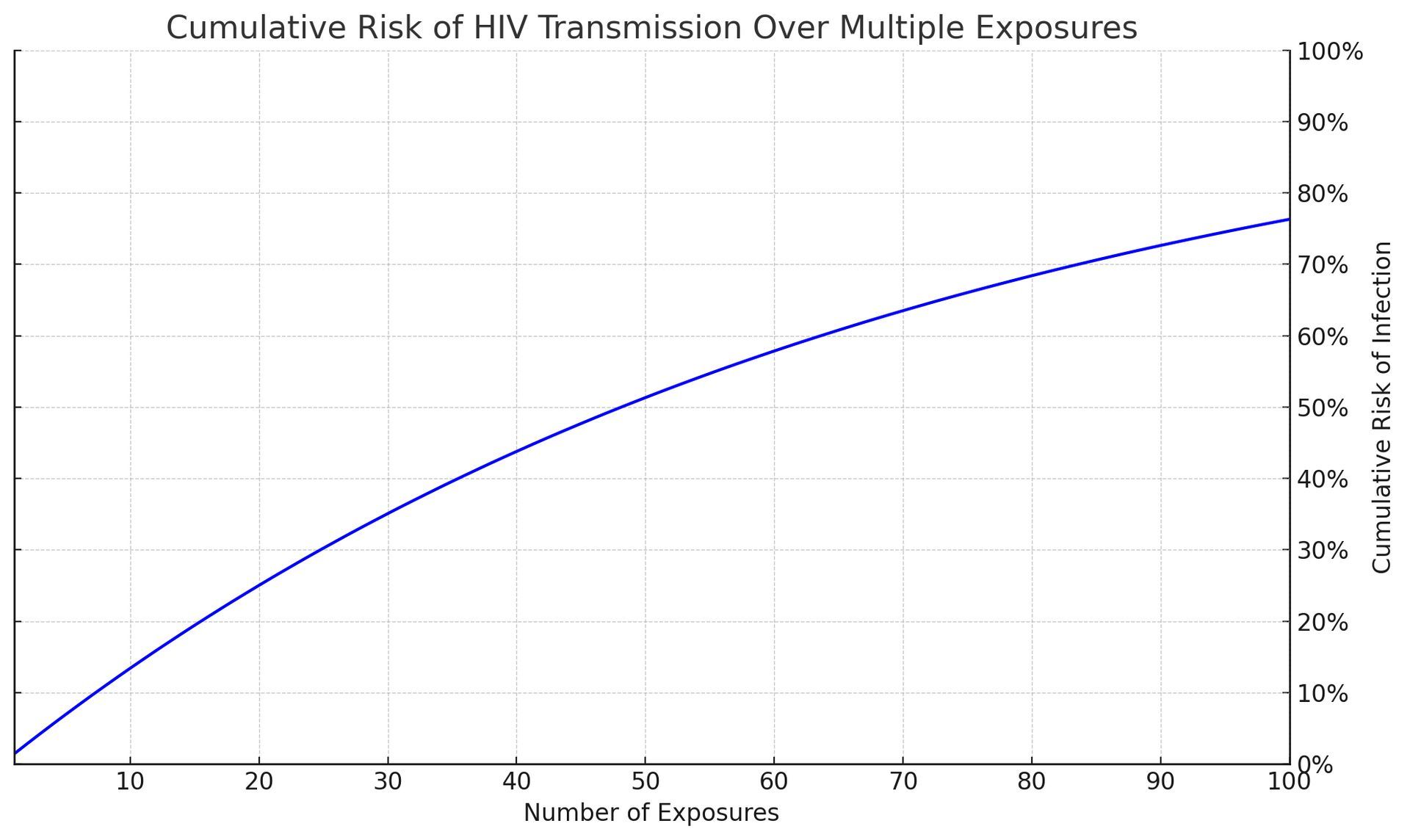
The chart above graphically demonstrates the escalating cumulative risk of HIV transmission correlating with an increase in exposures. Yes, the chances getting HIV from a one night stand is 1.43% but the danger compounds with each additional exposure.
With each successive exposure, the cumulative risk escalates markedly. This visual serves as a compelling reminder of why unwavering adherence to preventive measures is crucial, even in the face of seemingly minimal individual act risks.
It drives home the critical insight that risk from a single exposure, while modest, does not simply vanish with each new encounter. Rather, it builds, layer by layer, underscoring the imperative for consistent protective measures like condom usage and PrEP.
For those who delight in the precision of mathematics, here's the equation used by statisticians:
1−(1−per act risk)n
Where: per act risk = 1.43%
Employing this formula reveals the stark reality of how transmission risk intensifies with the accumulation of exposures. Whether it's after 10, 50, or even 100 encounters, the cumulative probability of HIV transmission climbs alarmingly, underscoring the importance of continuous vigilance in protection strategies.
| Number of Partners | Cumulative Risk |
|---|---|
| 1 | 1.43% |
| 5 | 6.86% |
| 10 | 13.08% |
| 20 | 24.56% |
| 50 | 53.57% |
| 100 | 76.32% |
The Snowball Effect:
How Multiple Partners Amplify Your 1.43% HIV Risk
You might be wondering, "If every hookup comes with a 1.43% chance of HIV, doesn't that number stay put, no matter how many people I'm with?" Say you've got five partners over three months. Each roll of the dice is 1.43%, right? So why doesn't that 1.43% just stick around, steadfast and unchanging?
That's a really good question.
To get why that 1.43% doesn't just hang tight, we need to dive into how cumulative risk plays out in the real world, not just on paper.
Let's think of it like a game of chance. Picture this: every time you play, there's a 1.43% chance you'll pull the short straw. The first time you play, sure enough, your chance of getting that straw is 1.43%. But here's where it gets tricky: every game is a new shot, with that same 1.43% chance. The game doesn't care about your past plays; each round is a fresh start.
Now, let's say each partner is a new game round. Having a month between partners doesn't zero out your risk slate. Every time you're intimate, it's like playing another round, each with its own 1.43% chance of drawing the short straw.
It's all about the buildup of risk over separate events. Each act might start with the same risk, but string a bunch of these acts together, and your overall chance of running into trouble at least once starts to climb.
Don't look at it simply as the chance of getting HIV from one exposure
It's kind of like crossing a busy road. Cross once, and your risk is pretty small. But keep crossing back and forth, and your chance of a close call goes up. Not because each crossing is riskier, but because you're putting yourself in harm's way more often.
So, even with breaks between partners, each one is like a new game round, bringing its own 1.43% chance to the table. As you add more partners into the mix, these separate risks stack up, nudging your overall chance of encountering HIV higher. This is why sticking to protective measures every single time is so crucial, no matter how much time passes between partners. It's about keeping those cumulative odds in check.
Conditions That Amplify HIV Transmission Risk By 500%
That 1.43% chance of catching HIV "per act" might look tiny at first glance, right? You might be thinking, "So, there's less than a 2% chance I could get HIV from one night? Awesome!"
Or maybe you're on the flip side, pondering, "Hang on, so there's a whopping 98.57% chance I won't get HIV even in a risky scenario?"
Hold off on popping the champagne just yet, because there's a twist to this story.
That 1.43% figure, while not wrong, doesn't tell the whole tale. It's an average, and averages have a sneaky way of glossing over the nitty-gritty details that could make a world of difference to you personally.
It Isn't just About The Chances of Contracting HIV After One Exposure
Here's the deal: that reassuring percentage might not hold up in every situation or for every person. Let's dive into why putting all your trust in this one number might be a bit misleading, especially when other factors like viral load and other sexually transmitted infections (STIs) come into play.
Think of it like this: if you're planning a day out and hear there's a 10% chance of rain, you might not bother with an umbrella. But if dark clouds are looming right above you, that umbrella suddenly seems like a good idea, doesn't it? Just like with the weather, knowing what can crank up your risk of HIV from a light sprinkle to a full-on storm is key in staying safe.
Viral Load Dramatically Increases The Risks
Imagine that each HIV-positive individual carries a metaphorical "bag of seeds." Each seed symbolizes a viral particle of HIV. The size of the bag and the number of seeds it holds can vary significantly from person to person, depending on their viral load. A larger bag filled with seeds signifies a high viral load, while a smaller bag with fewer seeds represents a lower viral load.
The Act of Scattering Seeds: Sexual Transmission
Think of each sexual encounter as an opportunity to scatter seeds from this bag. In this metaphor, the act of scattering seeds parallels the potential for HIV transmission. When a person with a high viral load (a large, full bag of seeds) engages in unprotected sexual activity, the odds of seeds being scattered—and taking root—are significantly higher with each encounter.
Essentially, the "per act" odds of transmission increase because there are more viral particles that could potentially be transferred to the sexual partner.
Experts reckon a packed viral load could crank up your risk of catching HIV by 3 to 5 times. That means instead of the 1.43% risk we've been chatting about, you could be looking at a risk that's anywhere from 4.29% to 7.15%. Let's split the difference and call it a 5.2% risk per encounter for simplicity.
Assuming a 5.2% "Per Act" Risk Factor
(midpoint between the range of 4.29% and 7.15%)
Take a look at what happens to the chances of getting infected with HIV when you take a top's high viral load into account:
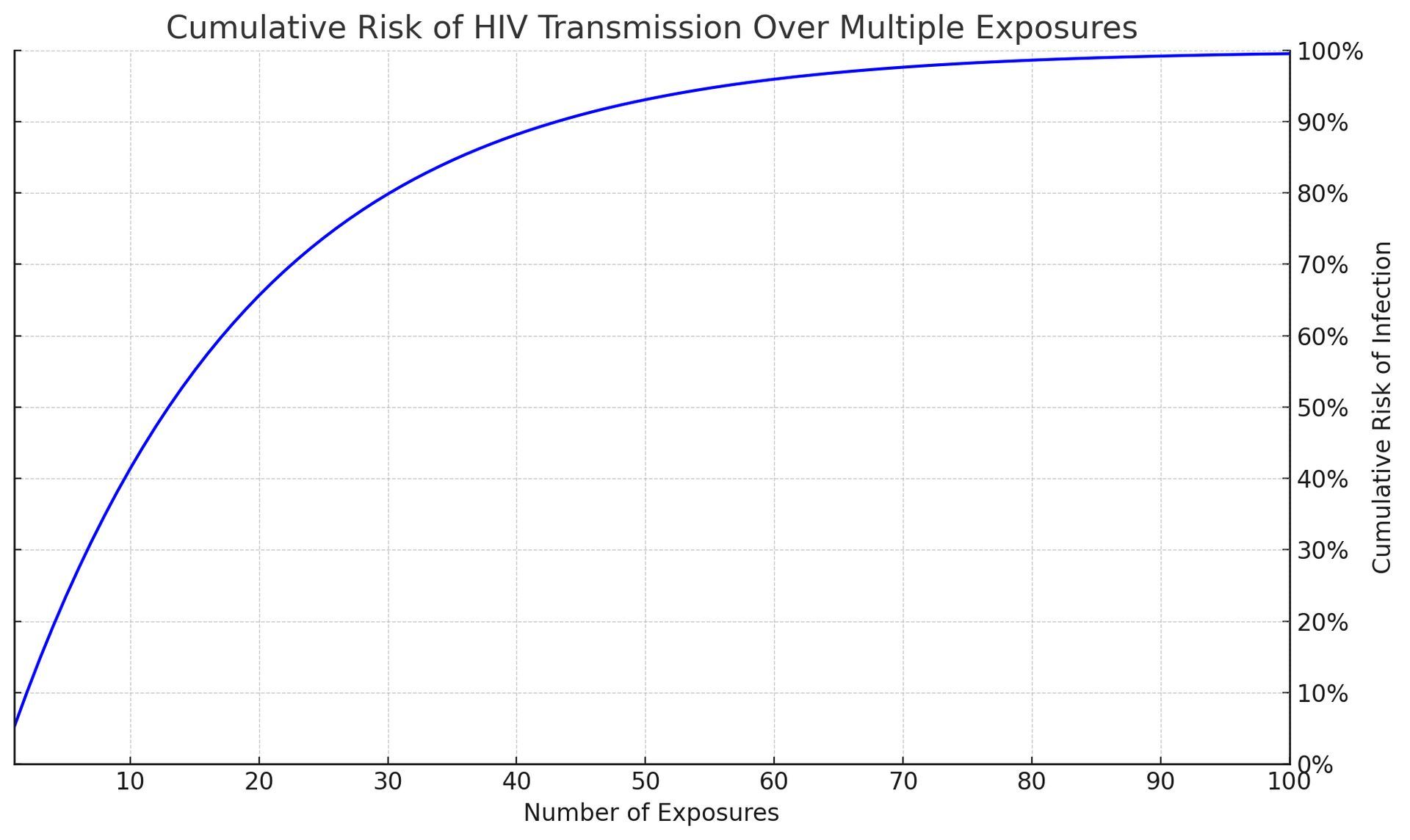
Remember how we talked about the average chance of getting HIV from a one-night fling being about 1.43%? Well, strap in, because things get a whole lot hairier when the person you're with has a high viral load.
Suddenly, we're not talking about 1.43% anymore; we're looking at a whopping 5.2% chance per hookup.
This isn't just about numbers on a page; it's about real risk stacking up with every encounter. Think of it as the risk compounding like interest in a bank, only what it's adding up to is anything but money in the bank.
Every time you go for an unprotected round with that kind of viral load in play, you're not just rolling the dice once; you're adding more dice to the game. And let me tell you, those dice can add up to a risk that's too big to ignore.
Sexually Transmitted Infections: The Fuel To HIV's Fire
Introducing STIs into the HIV equation is like pouring gasoline on an already smoldering fire—it dramatically intensifies the situation. An STI doesn't just nudge the risk up a notch; it catapults it. The inflammation and microscopic tears from STIs roll out the red carpet for HIV, slashing through your body's natural defenses with ease.
When you're dealing with an untreated STI, that seemingly manageable 1.43% risk per encounter? Forget about it. You're now in the territory of 2.86% to a staggering 7.15% risk each time. It's like each encounter is a spark, and with STIs in the picture, you're surrounded by kindling.
Now, think about combining a high viral load with the presence of STIs. It's like a small campfire suddenly facing a windstorm while doused in fuel—what was once contained is now a potential inferno. The risk isn't just growing; it's exploding, turning what might have been a cautious walk through the woods into a high-stakes race through a forest ablaze.
What is The Combined Impact of High Viral Load and STIs on HIV Transmission Odds?
Gird yourself and keep scrolling.
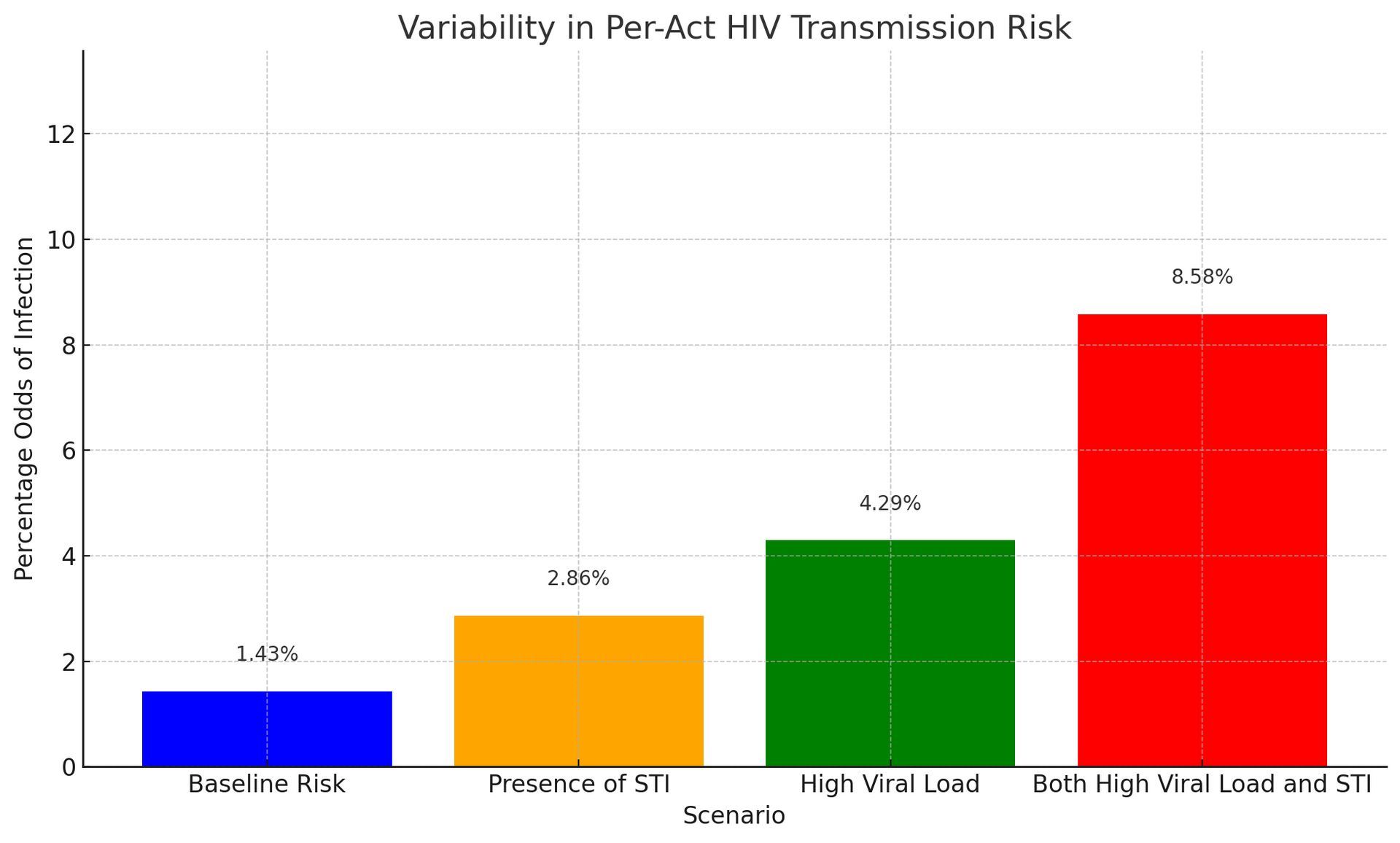
Imagine a graph where we kick off at the baseline HIV risk of 1.43%. From there, we step it up, layering in the game-changers: first an STI, then a high viral load, and finally, the double whammy of both together.
This isn't just a climb; it's a revealing journey that shows how quickly the odds of getting HIV from just one night can escalate. Each step up paints a vivid picture of risk building upon risk, culminating in a stark visual of what happens when these factors team up. It's a powerful snapshot of how each element boosts your risk and how, when combined, they amplify the stakes dramatically.
In real-life situations, the odds of HIV infection from one encounter can be around 1.43% on average. But, hold on tight, because depending on those factors we chatted about, it can skyrocket to a whopping 8.58% or even more.
Suddenly, that initial 1.43% doesn't sound so low, right?
The chart above shows the odds for just one encounter. But what happens when you have more than one? What about 5, 10, even 100 encounters? How does the cumulative effect of meeting people with STIs and high viral loads affect your chances of getting infected? Let's find out."
The Impact of Multiple Partners, STIs, and High Viral Load on HIV Risk
Below you'll see a table that meticulously outlines the HIV infection probabilities for a range of partner counts, from one to twenty. This analysis covers scenarios such as Baseline Risk, Presence of STI (Sexually Transmitted Infection), High Viral Load, and the amalgamation of Both High Viral Load and STI.
Please utilize the right-side scroller to navigate through this data:
| # of Partners | Baseline Risk | Presence of STI | High Viral Load | Both High Viral Load and STI |
|---|---|---|---|---|
| 1 | 1.43% | 2.86% | 4.29% | 8.58% |
| 2 | 3% | 6% | 8% | 16% |
| 3 | 4% | 8% | 12% | 24% |
| 4 | 6% | 11% | 16% | 30% |
| 5 | 7% | 14% | 20% | 36% |
| 6 | 8% | 16% | 23% | 42% |
| 7 | 10% | 18% | 26% | 47% |
| 8 | 11% | 21% | 30% | 51% |
| 9 | 12% | 23% | 33% | 55% |
| 10 | 13% | 25% | 35% | 59% |
| 11 | 15% | 27% | 38% | 63% |
| 12 | 16% | 29% | 41% | 66% |
| 13 | 17% | 31% | 43% | 69% |
| 14 | 18% | 33% | 46% | 72% |
| 15 | 19% | 35% | 48% | 74% |
| 16 | 21% | 37% | 50% | 76% |
| 17 | 22% | 39% | 53% | 78% |
| 18 | 23% | 41% | 55% | 80% |
| 19 | 24% | 42% | 57% | 82% |
| 20 | 25% | 44% | 58% | 83% |
How To Interpret This Table
The numbers in this table tell a sobering story about HIV risk that we cannot afford to ignore. At first glance, a 1.43% chance of infection from a single partner seems negligible - just a drop in the bucket, right? But as we trace the trajectory from one partner to twenty, that trickle becomes a flood.
With every new sexual encounter, the risk compounds exponentially. By partner number twenty, the baseline probability has skyrocketed to a startling 25% - a roll of the dice that no one should take lightly. The backdrop suddenly shifts from nonchalant to ominous.
But the real twist comes as we factor in the combustible elements of an STI and high viral load. These are the sparks that can ignite an outright inferno of risk. Just one lit match in the form of an STI doubles the starting odds to nearly 3%. By partner twenty, the chances of escaping uninfected plummet to just over half at 56%. The outlook turns grim.
Now add the accelerant of a high viral load. This is the combination that turns the spark into a five-alarm fire, with the odds leaping to a staggering 83% by partner twenty. These multiplying variables tell a harrowing story of how HIV transmission can spiral out of control if left unchecked.
The numbers don't lie. This table shouts a warning that we need to heed if we want to alter the HIV narrative. It shows how easily manageable risk can transform into grave danger when compounded over time.
What Are Your Chances of Getting HIV from a Needle Poke?
The CDC paints a concerning picture, estimating that the per-act risk of HIV transmission through needle sharing among people who inject drugs can be as high as 0.63%. This heightened risk is a result of direct blood exchange, often containing a substantial viral load, which facilitates efficient virus transfer.
Beyond Needles: Continued Risks
However, the danger extends beyond needles alone. Sharing other drug paraphernalia, such as cookers, cotton, or water, may carry slightly lower risks compared to direct needle sharing, but they still involve the potential mixing of blood and bodily fluids. These actions create pathways for HIV transmission that demand attention.
An Unexpected Finding
Here's a jarring revelation: The act of having a penis inserted into your rectum carries a higher risk of HIV infection than sticking yourself with a needle contaminated with blood! It's a pretty perplexing thought, isn't it? Let's take a closer look at this intriguing finding.
Unprotected Anal Sex Poses Higher HIV Risk Than Blood-Contaminated Needle Use
Unprotected Anal Sex vs. Blood-Contaminated Needle: Who Would've Guessed?
It's quite the eyebrow-raiser, isn't it? The risk of contracting HIV per encounter during receptive anal sex stands higher at 1.43% compared to a seemingly shocking 0.63% from something as nerve-wracking as injecting yourself with a needle previously used by someone else.
It's the kind of revelation that makes you go, "Wait, really?" Let's break it down into bite-sized pieces to unravel why this intriguing contrast exists.
The Vulnerable Backdoor:
First off, the lining inside your rectum is incredibly thin and prone to small tears. It's like an open invitation for HIV to make its way into your bloodstream. Plus, this region is teeming with immune cells that HIV finds quite appealing. So, despite appearances, unprotected anal sex is akin to rolling out the red carpet for HIV.
The Needle's Secret:
Now, onto the needle scenario. You'd assume that sharing a needle would be a direct blood swap and therefore immensely risky, right?
Well, here's the twist: not every needle contaminated with someone else's blood carries enough HIV to trigger an infection. Furthermore, the amount of blood transferred by a needle is minuscule. Plus, some individuals who use needles might clean them thoroughly or have access to clean ones, significantly reducing the risk.
The Viral Load Variable:
But hold on, there's more to the story! Enter the concept of viral load—a fancy term for the quantity of HIV in someone's blood. If an individual consistently takes their HIV medications and maintains a low viral load, the likelihood of transmitting the virus drops significantly, even if they accidentally share a needle.
Frequency and Context Matters:
Consider this: if more people engage in unprotected sex than share needles, it logically follows that more HIV transmissions occur through sexual encounters. Additionally, individuals might take measures to mitigate risks when sharing needles, such as participating in needle exchange programs.
Biology's Role:
Last but not least, let's revisit the biology of it all. Your skin and the underlying tissues are quite resilient, making it tougher for a needle to introduce HIV into your system. In contrast, anal sex provides a more straightforward path for the virus to reach its destination.
Yes, it's indeed true—the chances of contracting HIV from a needle prick are significantly lower than from unprotected receptive anal sex.
What Are the Odds of Catching HIV from a Blood Transfusion?
In places with top-notch blood testing, like the U.S. and other well-off countries, getting HIV from a blood transfusion is super rare.
We're talking about a tiny chance, roughly 1 in 1.5 million transfusions, or a minuscule 0.000067% per transfusion. That's incredibly low, and it's all thanks to some serious science in the form of nucleic acid testing (NAT). This kind of testing is super sharp at picking up HIV way earlier than the older tests that looked for antibodies.
But let's not sugarcoat it - in parts of the world where the blood doesn't get such a thorough check-up, the risk shoots up dramatically. Back in the day, before blood screening became a thing everywhere, the risk of catching HIV from a transfusion with infected blood was a staggering 90-95%. Basically, if the blood was infected, it was almost a sure bet the recipient would get HIV too.
It's worth mentioning that these odds can change depending on how rigorously the blood is screened and how common HIV is among donors in that area. Thanks to the solid blood safety practices in places like the U.S., the risk has been slashed to nearly nothing, marking a huge win in the ongoing fight to stop HIV in its tracks.
How Experts Determine Your Chances of Catching HIV
Methods of HIV Risk Assessment
In the realm of HIV risk evaluation, scientists employ various methods to arrive at essential numbers that guide our understanding. Let's delve into these methodologies:
1. Cohort Studies
Cohort studies are the backbone of HIV risk research. They involve tracking groups of individuals over time to observe HIV transmission under different circumstances. These studies provide insights into per-act risk for various sexual activities. However, they demand significant time and resources and may introduce biases.
2. Case-Control Studies
Case-control studies compare individuals who have contracted HIV with those who haven't. They look back in time to determine exposure levels to different risk factors. These studies offer quick insights but may be influenced by recall and selection biases.
3. Mathematical Modeling
Mathematical models simulate the complex factors affecting HIV transmission. They can incorporate data from various sources to estimate risks under different scenarios. Models are useful for exploring hypothetical situations and predicting trends but rely on the quality of input data and assumptions.
These methodologies form the foundation for understanding and quantifying HIV risk.
Approaches to Trustworthy HIV Risk Estimation
In the realm of HIV risk estimation, no single method is considered an isolated "gold standard." Each approach contributes unique strengths to our understanding of HIV risks. When findings from different methods align, confidence in the results grows.
Cohort Studies: The Observational Pillars
Cohort studies, with their direct, long-term observation, hold substantial weight in risk assessment. When supported by case-control studies and mathematical models, the consistency across diverse research approaches enhances the credibility of risk estimates.
Understanding the Science
Understanding the science of HIV risk estimation is not merely an academic exercise; it's a practical tool for informed decision-making. By comprehending how researchers derive these numbers, we can better interpret their implications for our lives. Whether a statistic offers reassurance or caution, it empowers us to make informed choices for our health and well-being.
Navigating HIV Risk
In our journey through the intricacies of HIV risk, it's crucial to recognize that behind each statistic lies rigorous scientific inquiry aimed at guiding safer sexual health decisions.
These adjustments emphasize the variability in risk and the influence of individual factors on transmission probabilities. They underscore the importance of protective measures such as condoms and PrEP, even when the baseline per-act risk appears low.
Other Ways You Can Get HIV Sexually
Kissing: Minimal HIV Risk
Casual kissing poses no significant risk of HIV transmission. The virus cannot be transmitted through saliva alone, and the viral quantity in saliva is typically insufficient to pose a threat. However, deep or "French" kissing may carry a minimal risk if there are open sores or bleeding gums in the mouth, though such instances are exceedingly rare and poorly documented.
Mutual Masturbation: Low HIV Risk
Mutual masturbation is generally safe concerning HIV transmission. The risk is minimal unless open wounds on the hands or genitals come into direct contact with HIV-infected bodily fluids.
Use of Sex Toys: Risk Depends on Hygiene
The risk associated with using sex toys hinges on whether they are shared and their cleanliness. Sharing sex toys without proper cleaning or using new condoms each time can pose a risk if the toys are contaminated with HIV-positive blood, semen, or vaginal fluids. Thorough cleaning or using barriers like condoms on sex toys can significantly reduce this risk.
Online HIV Chance Calculators
Online Tools for HIV Risk Assessment
In the digital era, online tools and HIV chance calculators have become valuable resources for individuals seeking to assess their risk of HIV transmission.
These tools, ranging from simple calculators to comprehensive risk assessment applications, provide a means to evaluate potential risks based on individual behaviors and situations. Let's delve into the world of these online resources, examining their accuracy, usefulness, and where to find the most reliable options.
Diverse Range of Calculators
Online HIV risk calculators come in various levels of complexity and factors they take into account. Basic calculators may inquire about sexual behavior, condom use, and the partner's HIV status to offer a rough risk estimate.
Advanced tools consider a broader spectrum of variables, encompassing the type of sexual activity, frequency, drug use, and even geographical location, considering varying HIV prevalence rates in different regions.
If you're looking for the odds of contracting HIV after one exposure these calculators can help. They typically draw on data from epidemiological studies and HIV transmission risk research to generate personalized risk assessments. By inputting specific behaviors and circumstances, users can obtain an estimate of their HIV risk for a given encounter or over a specified period. Here are 4 we like:
Centers For Disease Control (CDC)
Northwestern University HIV Risk Calculator
Assessing Accuracy and Utility of HIV Chance Calculators
The accuracy of online HIV risk calculators hinges on various factors, including data quality and the comprehensiveness of the questions they pose. Calculators relying on current research and considering a broad array of behaviors and factors tend to be more dependable.
However, it's essential to acknowledge the inherent limitations of these tools. They can provide risk estimates but cannot encompass every possible variable or individual circumstances.
The utility of these calculators lies in their capacity to raise awareness and encourage individuals to contemplate their behaviors and potential risks. They serve as an excellent starting point for discussions about safer sex practices and the importance of regular HIV testing.
Nevertheless, they should not substitute professional medical advice or serve as the sole basis for sexual health decisions.
Should You Get Post-Exposure Prophylaxis After a Night With an HIV Top?
Imagine you've just had a night that's turned your world upside down. You find out that your one-night stand was HIV positive, and now you're faced with a whirlwind of emotions and decisions.
The clock is ticking on a decision about Post-Exposure Prophylaxis (PEP), and you're armed with a statistic from the NIH and CDC: the odds of getting HIV from one exposure is 1.43%. You're wondering,
"Is it really worth going through the hassle and discomfort of PEP for such a small chance?"
Let's break it down together, shall we?
Understanding the 1.43% Statistic
First off, that 1.43% figure might seem small, but it's not negligible. Think of it as a little over 1 in 100 chance. If you were told there was a 1 in 100 chance of rain, you might still grab an umbrella, right? HIV is far more serious than getting caught in the rain, so even a small percentage represents a risk worth considering seriously.
What's PEP, Anyway?
PEP is like the morning-after pill but for HIV exposure. It's a course of antiretroviral medicines that, if started within 72 hours of exposure, can significantly reduce your risk of becoming infected.
The key is timing—the sooner, the better. It's like putting out a fire before it spreads; PEP works to stop the virus in its tracks before it takes hold in your body.
Weighing the Costs and Benefits
PEP isn't a walk in the park. It involves a month of medication, and these drugs can pack a punch with side effects like nausea, fatigue, and headaches for some people.
Then there's the cost and the time commitment to consider. But let's put this into perspective: these temporary discomforts are a preventive measure against a lifelong condition that requires ongoing management and can significantly impact your quality of life.
Making the Decision
Understanding the nuances of your situation can significantly influence your decision-making process. Let's explore some circumstances that might sway your decision, using a warm and conversational tone to unpack these complex considerations.
Scenario 1: The HIV Positive Partner is on Medication with an Undetectable Viral Load
If you know that the HIV-positive partner is on antiretroviral therapy (ART) and has an undetectable viral load, this information can be quite comforting. An undetectable viral load means the amount of HIV in the blood is so low that it can't be detected by standard tests.
Studies have shown that individuals with an undetectable viral load effectively have no risk of transmitting the virus to HIV-negative partners through sex.
Furthermore, if you're confident that the partner does not have any other sexually transmitted infections (STIs), this further reduces the risk. STIs can inflame or break the skin, providing easy entry points for HIV, so their absence is another layer of reassurance.
Scenario 2: Unknown Medication Status and Potential STIs
On the flip side, let's say the partner was from out of town, and you have no way of confirming whether they're on medication or if they have any STIs. This uncertainty introduces a higher level of risk. Without the assurance of an undetectable viral load, you're left with the baseline statistics, where the 1.43% risk comes back into full view. The unknowns about STIs further complicate the picture, as their presence can amplify the risk of HIV transmission.
In such a scenario, the decision to undergo PEP might lean more towards a 'yes.' The absence of detailed information about the partner's HIV management and STI status introduces significant unknowns, and in the face of uncertainty, erring on the side of caution is a common and understandable choice.
Scenario 3: The HIV-Infected Partner is Not on Medication and Has an STI
In this scenario, we're navigating even more turbulent waters. When the HIV-positive partner is not on medication, meaning their viral load is potentially high, the risk of HIV transmission increases.
Antiretroviral therapy (ART) plays a critical role in managing HIV, reducing the viral load to undetectable levels and significantly lowering the chance of transmission. Without this treatment, the virus is more active in the body, and the risk of passing it on during an encounter rises above the baseline 1.43%. Way above, to 4.29% (see chart above).
Adding the presence of an STI into the mix further amplifies this risk--up to 8.58%. STIs can cause sores or inflammation in the genital area, compromising the integrity of the skin or mucous membranes, and providing a direct pathway for HIV to enter the body. This is particularly concerning because even without the consideration of HIV, STIs can be a significant health issue that requires treatment.
Weighing the Decision for PEP in Scenario #3
In this third scenario, the argument for considering PEP becomes stronger. The increased risk due to the absence of ART in the HIV-positive partner and the additional risk factor of an STI makes the potential exposure more concerning. It's a situation that tilts the scales towards taking preventive action to protect your health.
The Importance of Immediate Action
Time is of the essence when it comes to PEP. The treatment is most effective when started as soon as possible, ideally within 24 hours and no later than 72 hours after potential exposure. Given the heightened risk in this scenario, seeking immediate medical attention not only for the consideration of PEP but also for advice and treatment for potential STI exposure becomes even more critical.
Comprehensive Care
In this scenario, it's also vital to address the STI, regardless of the decision about PEP. STIs can have long-term health implications if left untreated, and addressing them promptly is important for your overall well-being.
Scenario 3 presents a situation with heightened risk, where the absence of ART in the HIV-positive partner and the presence of an STI contribute to a more significant concern for HIV transmission. In such cases, the consideration for PEP is stronger, and immediate consultation with healthcare professionals is crucial. They can provide a comprehensive risk assessment, initiate PEP if deemed appropriate, and address the STI, ensuring a holistic approach to your health in the wake of potential exposure.
Navigating the Decision Considering All 3 Scenarios
These contrasting scenarios highlight the importance of personalized information in decision-making about PEP. The more you know about the specific circumstances of your exposure, the more tailored your risk assessment can be. However, in many real-life situations, complete information may not be available, and decisions must be made under uncertainty.
Conclusion
Deciding whether to undergo PEP is deeply personal and can be influenced by a variety of factors, including the specifics of the HIV exposure, the information available about the partner's HIV status and management, and the presence or absence of other STIs. In scenarios where detailed information is not available, the decision might lean more towards precautionary measures.
Ultimately, the choice to undergo PEP should be made after careful consideration of all available information, personal risk tolerance, and consultation with healthcare professionals. It's about weighing the potential benefits against the costs and side effects, all while navigating the emotional and psychological landscape that comes with such a significant health decision.